Pharmacokinetics Important Notes
- Pharmacokinetics
- It is the study of drug absorption, distribution, biotransformation, and excretion
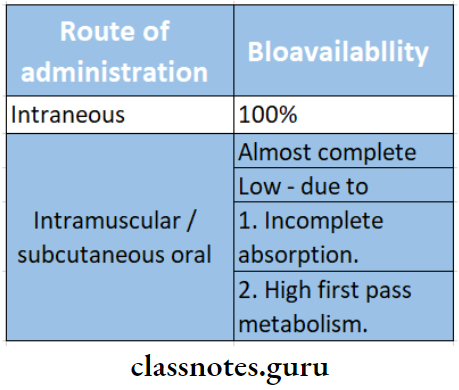
- Bioavailability
- It is the amount or percentage of drug that is absorbed from a given dosage form and reaches the systemic circulation following nonvascular administration
- Biotransformation
- It is the alteration of a drug within living organisms
- After absorption drug circulates in the blood either in free form or bound to plasma proteins
- The protein-bound drug is inactive and acts as a temporary store
- The liver is the most active site for metabolizing the drugs
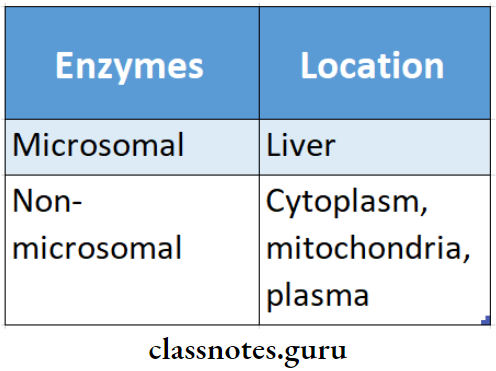
- The enzymes that bring about biotransformation are microsomal enzymes
- Routes of excretion of the drug
- Lungs – alcohol, paraldehyde
- Skin – arsenic, heavy metals
- Bile – erythromycin, tetracycline, glycosides
- Milk – erythromycin, tetracycline, penicillin
- Saliva – metronidazole, heavy metals
- Tears – rifampicin, minocycline
- First order kinetics
- Elimination of a drug occurs exponentially
- A constant fraction of the drug disappears in each equal interval of time at the rate proportional to its plasma concentration
- It occurs in lower dosage levels
- Zero-order kinetics
- When the dose exceeds a certain critical level, eliminating mechanism gets saturated
- A fixed quantity of drug is eliminated per unit of time
Alcohol effects on health questions and answers
- Methods of prolonging drug action
- Retarding absorption
- Inhibiting drug metabolism in the liver
- Slowing renal excretion of the drug
- Increased protein binding of the drug in plasma
- Drugs are transported across the membrane by
- Passive diffusion and filtration
- Specialized transport
- Drug dosage
Read And Learn More: Pharmacology Question and Answers
\(\frac{\text { Child weight (in lbs) }}{150} \times \text { adult dose }\)
\(\frac{\text { Age of child }}{\text { Age }+12} \times \text { adult dose }\)
Pharmacokinetics Long Essays
Question 1. Describe the various methods to prolong the duration of action of the drug.
Answer:
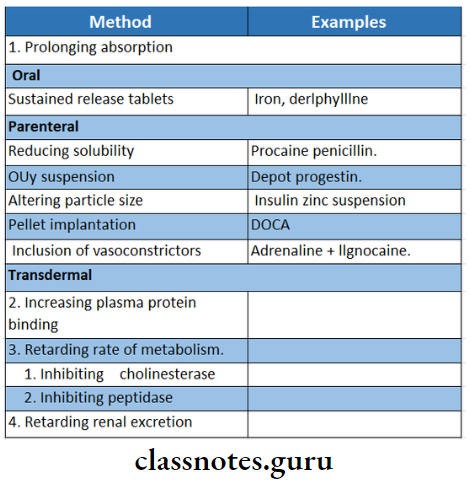
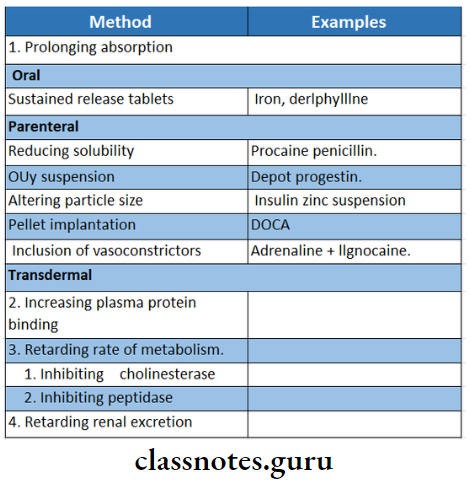
The duration of action of drugs can be prolonged by in-interfering with the pharmacokinetic processes.
- It has the following advantages:
- Reduces frequency of drug administration.
- Improves patient compliance.
- Avoids large fluctuations in plasma concentration.
- Maintains drug effect overnight.
Prolong The Duration Of Action Of The Drug Methods:
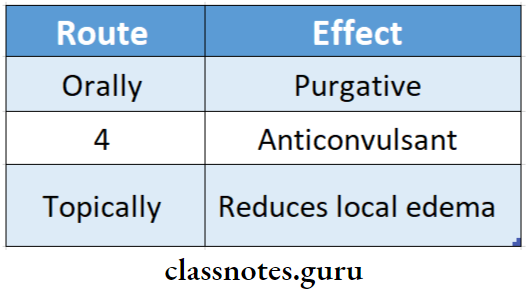
1. By prolonging the absorption:
- The oral route prolongs absorption by 4-6 hours.
- Used sustained-release preparation, coating with resin, plastic, etc. Temporarily disperse the release of the active ingredient in the GIT.
- Used the semipermeable membrane to control the release of the drug.
- Example: Iron, dyphylline.
- Parenteral route – prolongs absorption up to days to several months.
- Reducing solubility – Example: procaine + penicillin.
- Use of oily solution depot progression.
- Altering particle size – Insulin zinc suspension.
- Pellet implantation – DOCA.
- Statistic capsules – testosterone.
- Inclusion of vasoconstrictor with the drug adrenaline with local anesthetics.
- Combining with protein – protamine + zinc + in-caution.
- Chemical alteration through esterification.
- Transdermal drug deliver:
- Use of transdermal patch.
Alcohol-related diseases questions
2. By increasing plasma protein binding:
- Drugs that are highly bound to plasma protein are pre- pared & are released slowly in the free active form.
- Example: sulphonamides.
3. By Retarding the rate of Metabolism:
- By chemical alteration of drug – Example: addition of ethical group to estradiol.
- Inhibiting specific enzymes.
- Inhibition of enzyme cholinesterase by posting- mine prolongs the action of acetylcholine.
- Inhibition of enzyme peptidase in the renal tubules by cilastatin – prolongs the action of imipenem.
4. By Retarding Renal Excretion:
- Use of competitive substances, which competes for the same transport system.
- Example: Probenecid pro- longs the action of penicillin and ampicillin.
Question 2. Explain the means of biotransformation of drugs in the body with examples.
Answer:
Biotransformation:
- Biotransformation is the process of chemical alteration of the drug in the body.
- It converts the drugs into more polar, water-soluble compounds so that they are easily excreted through the kidneys.
Site of Biotransformation:
- Liver – most important organ.
- Other includes kidney, gut, mucosa, lungs, blood & skin.
Biotransformation Consequences:
- Inactivation.
- Active metabolites & drugs are converted to inactive or less active substances.
- Example: Lidocaine, ibuprofen.
- Active metabolite from an active drug.
- Activation of the inactive drug.
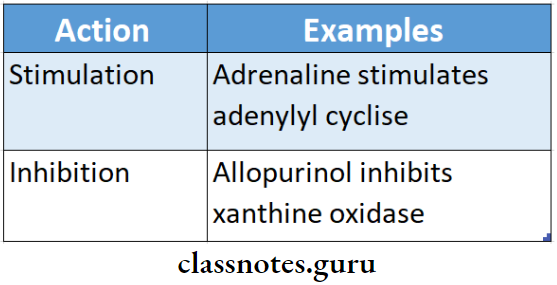
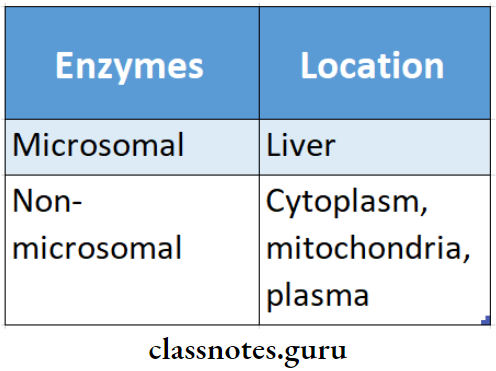
- Enzymes in biotransformation:
Alcohol use disorder questions and answers
Reactions in Biotransformation:
1. Phase 1 reactions or non-synthetic reactions.
It converts the drug to a more polar metabolite by oxidation, reduction, or hydrolysis.
- Oxidation.
- It involves the addition of oxygen or negatively charged radicals or either the removal of hydrogen or positively charged radicals.
- They are mostly carried out by a group of mono-oxygenases in the liver.
- They are the most important drug metabolizing reactions.
- Reduction.
- It involves cytochrome P-450 enzymes working in opposite directions.
- Hydrolysis.
- This cleavages of drug molecules by taking up a molecule of water.
\(\text { Ester }+\mathrm{H}_2 \mathrm{O} \stackrel{\text { esterase }}{\longrightarrow} \text { acid }+ \text { alcohol }\)
2. Phase 2 reactions or synthetic reactions.
- In it, endogenous water-soluble substances combine with the drug or its phase 1 metabolite to form a highly polar conjugate.
- Various synthetic reactions are:
- Glucuronide conjugation.
- It is a most important synthetic reaction.
- Carried out by a group of UDP-glucuronosyl transferases.
- Acetylation.
- Compounds having amino or hydrazine residues are conjugated with the help of acetyl cohen- zyme-A.
- Methylation.
- Amines & phenols can be methylated.
- Sulfate conjugation.
- Phenolic compounds & steroids are sulfated by sulfotransferases.
- Glycine conjugation.
- Salicylates are conjugated with glycine.
- Glutathione conjugation.
- Serves to inactivate highly reactive quinine or epoxide intermediates formed during metabolism.
- Ribonucleoside.
- Required for activation of many purine & pyrimidine antimetabolites used in cancer chemotherapy.
Pharmacokinetics Short Essays
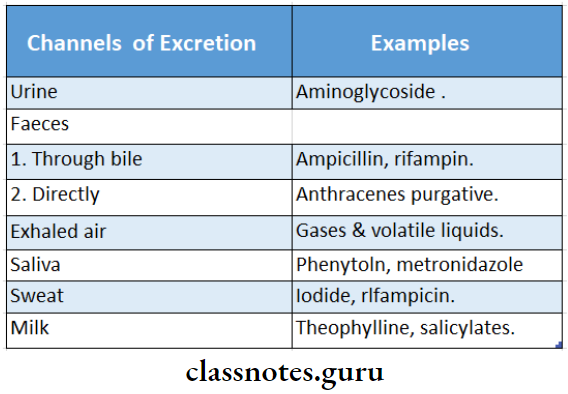
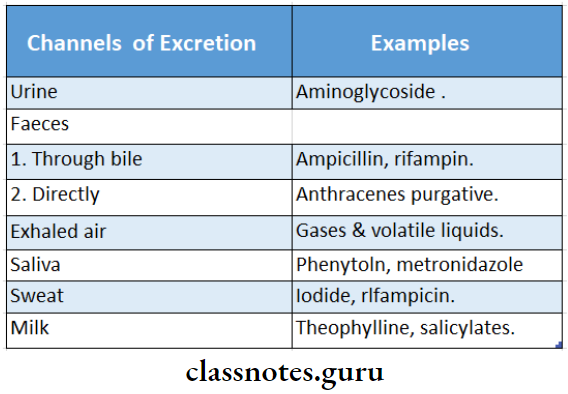
Question 1. Channels of drug excretion.
Answer:
Drug & their metabolites are excreted.
1. Urine.
- Through kidney.
- A most important channel for the majority of drugs.
- It takes place in three steps.
- Glomerular filtration.
- Ionized drugs of low molecular weight are easily filtered through the glomerular membrane.
- All nonprotein drugs are presented to the glomerulus for filtration.
- Tubular reabsorption.
- It depends upon lipid solubility & ionization of the drug at the existing urinary pH.
- Tubular secretion.
- It involves the active transfer of organic acids & bases by two separate classes of nonspecific transporters.
2. Faeces:
- Unabsorbed portions of the orally administered drugs are eliminated through the faeces.
- Most of the drug present in it is derived from bile.
- Certain drugs are excreted directly in the colon.
3. Exhales air:
- Gases & volatile liquids are eliminated by the lungs.
4. Saliva & sweat.
- Drugs like phenytoin and metronidazole are excreted through saliva.
- Drugs like iodide and rifampicin are excreted through sweat.
5. Milk.
- The excretion of drugs in the milk is of no significance to the mother, but the infant receives the drug during suckling.
Questions and answers on alcohol abuse
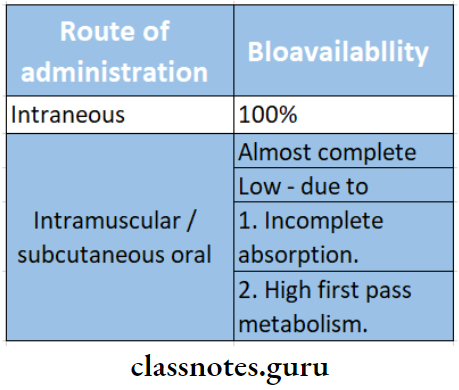
Question 2. First pass metabolism/Pre-systemic metabolism.
Answer:
First-pass metabolism is the metabolism of the drug during its first passage from the site of absorption into the systemic circulation.
- Most of the orally administered drugs have to pass via the gut wall, portal vein & liver to enter the systemic circulation.
- Certain drugs during this process of passage get metabolized & are removed or inactivated before they reach systemic circulation.
- This process is known as first-pass metabolism.
- Its extent depends on the individual & the drug.
- Bioavailability is increased in patients with hepatic diseases.
Result of first-pass metabolism:
- Decreases bioavailability of the drug.
- Decreases the therapeutic effect of the drug.
Pre-systemic metabolism Consequences:
- The dose has to be increased.
- The route of administration has to be changed.
Examples: Phenobarbitone has low first-pass metabolism & lidocaine has high first-pass metabolism.
Question 3. Bioavailability mentions factors influencing it by oral route with examples.
Answer:
Bioavailability:
- Bioavailability is the fraction of a drug that reaches the systemic circulation following administration by any route.
Factors influencing it:
- Disintegration & dissolution.
- Oral drugs have to be disintegrated to be absorbed & then dissolved in gastrointestinal fluids.
- Liquids → faster absorption→ good bioavailability.
- Formulation.
- Inert substances used with diluents’ slow absorption reduce bioavailability.
- Particle size.
- Small particles have easy absorption → better bioavailability.
- Lipid solubility.
- Lipid-soluble drugs- fast absorption → more bioavailability.
- pH & ionization.
- lionized drugs – poor absorption → less availability.
- Acidic drugs unionized and rapidly absorbed → good bioavailability.
- Area & vascularity of the absorbing surface.
- Larger area – more vascularity → more absorption → more bioavailability.
- Gastrointestinal motility.
- Faster gastric emptying → fast passage into the intestine → more absorption→ more bioavailability.
- Presence of food.
- Delayed gastric emptying → delay absorption.
- Metabolism.
- Degradation of drugs in GIT leads to zero bioavailability.
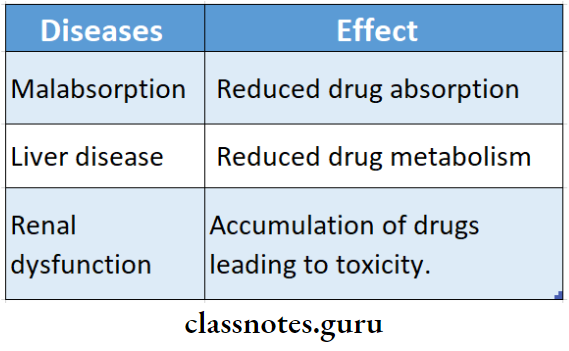
- Diseases.
- Liver diseases lead to increased bioavailability.
Question 5. Various methods to prolong drug action.
Answer:
1. By prolonging the absorption
- Oral route
- Prolongs absorption by 4-6 hours
- Used sustained-release preparation, coating with resin, plastic, etc
- Temporarily disperse release of the active in-gradient in the GIT
- Use of semipermeable membrane to control the release of drug
- Parenteral route
- Prolongs absorption upto days to several months
- Reducing solubility
- Use of oily solution
- Altering particle size
- Pellet implantation
- Siastic capsules
- Inclusion of vasoconstrictor with drugs like adrenaline
- Combining with protein
- Chemical alteration through esterification
- Transdermal route
- Use of the transdermal patch
2. By increasing plasma protein binding
- Drugs that are highly bound to plasma proteins are prepared and are released slowly in the free active form
3. By retarding the rate of metabolism
- By chemical alteration of drug
- Inhibiting specific enzyme
4. By retarding renal excretion
- Uses of competitive substances which compete for the same transport system
Alcohol pharmacology questions and answers
Pharmacokinetics Short Answers
Question 1. Pharmacokinetics.
Answer:
Pharmacokinetics is the study of the absorption, distribution, metabolism & excretion of drugs i.e., the movement of the drug into, within, and out of the body.
- Once a drug is administrated→ it is absorbed → enters blood distributed to different parts of the body → reaches the site of action metabolized and excreted out of the body.
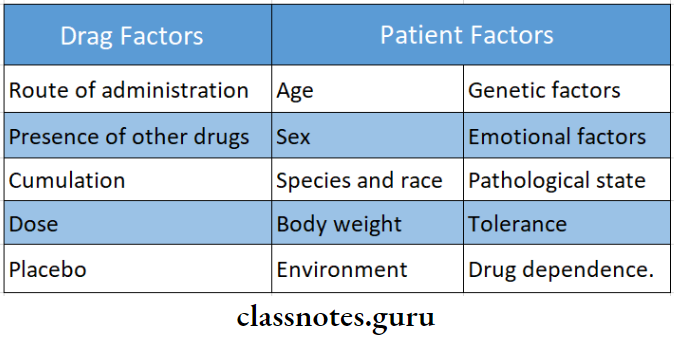
- It depends upon.
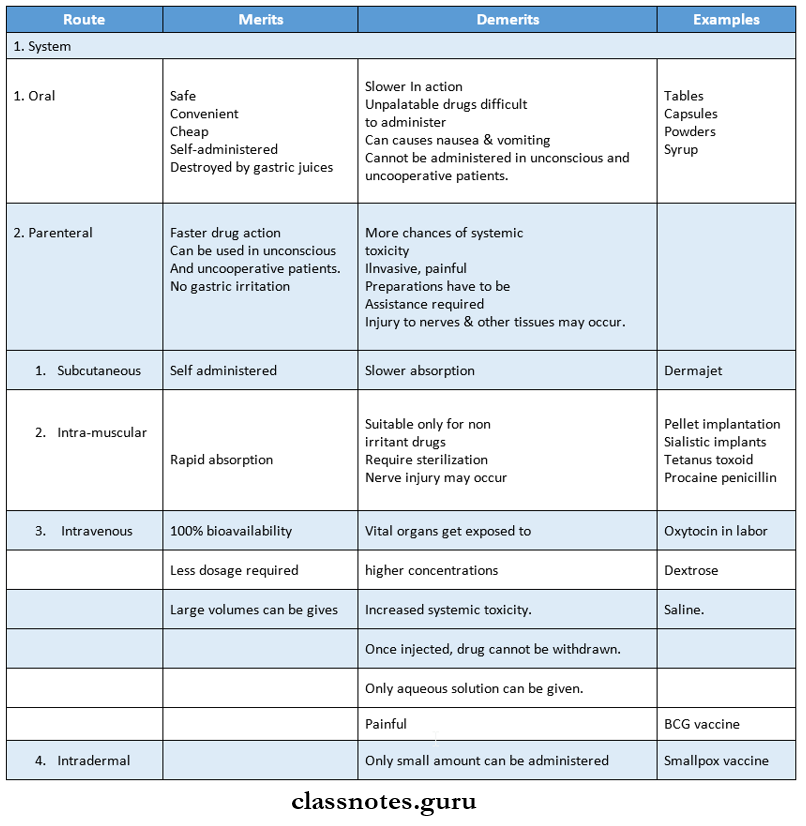
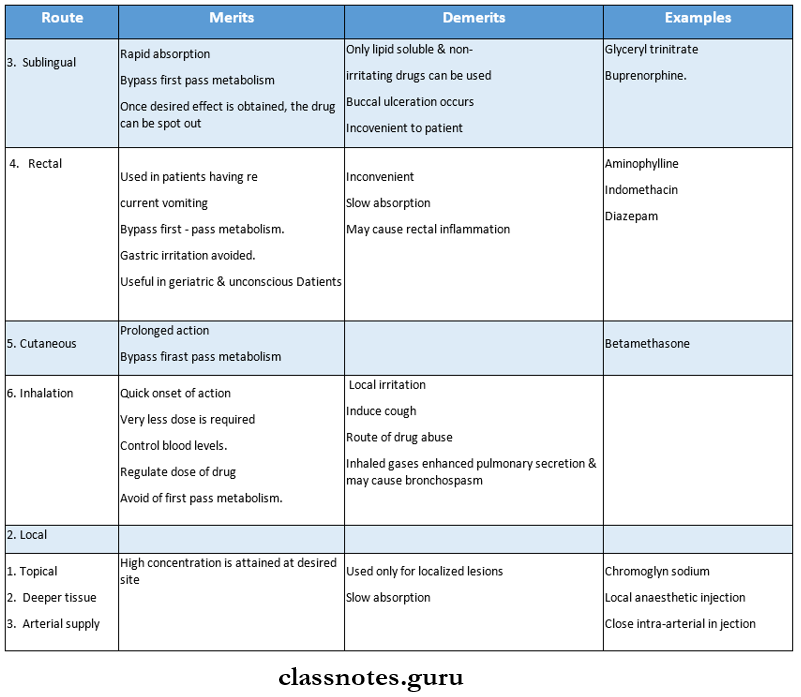
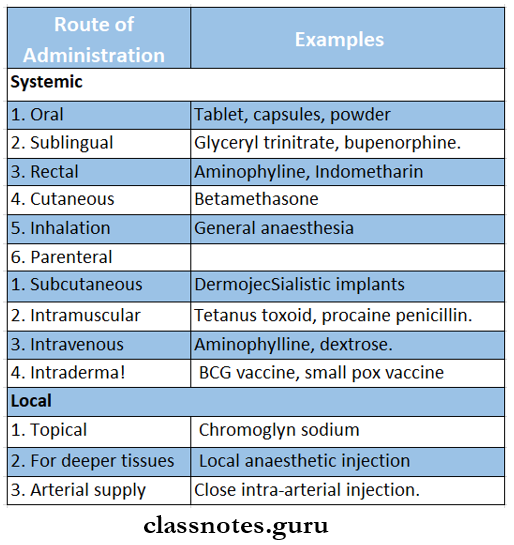
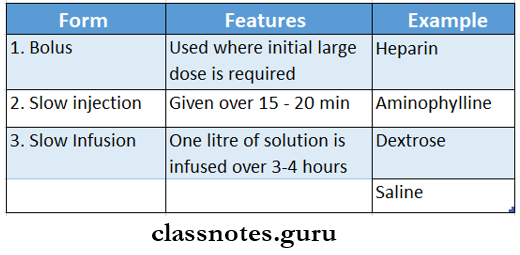
- Route of administration.
- Dose
- Latency of onset.
- Time of peak action.
- Duration of action.
- Frequency of administration.
Question 2. Mention factors affecting bioavailability.
Answer:
- Disintegration & dissolution of the drug.
- Formulation.
- Particle size.
- pH & ionization.
- Lipid solubility.
- Gastrointestinal motility.
- Presence of food.
- Metabolism.
- Area & vascularity of absorbing surface.
- Diseases.
Question 3. Mention channels of excretion of drug with examples.
Answer:
Questions on alcohol consumption and effects
Question 4. Methods of prolonging effects of the drug with examples.
Answer:
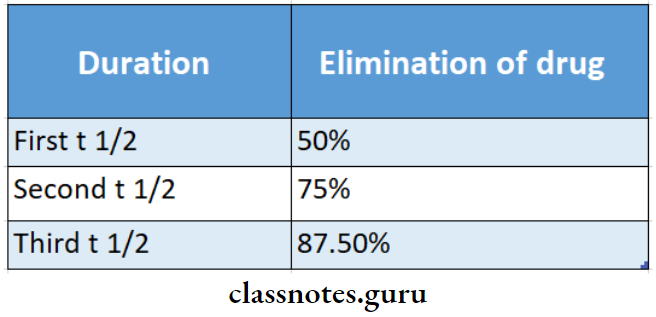
Question 5. Plasma half-life
Answer:
The plasma half-life (t1/2) of the drug is the time taken for its plasma concentration to be reduced to half its original value.
Plasma half-life Phase:
- Initial rapid phase.
- Declined phase.
- Occurs due to elimination.
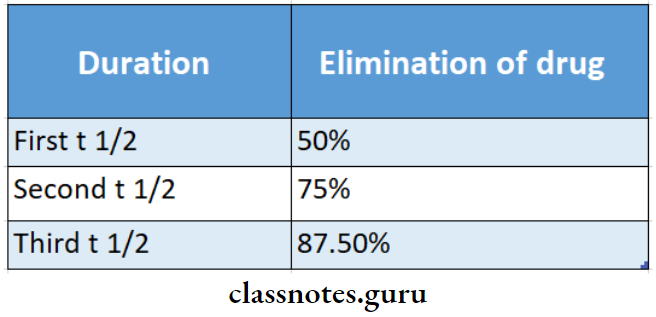
- Four to five half-lives are required for the complete elimination of the drug.
Plasma half-life Significance:
- Calculate the loading & maintenance dose of the drug.
- Indicates the duration of action of the drug.
- Guides dosing regimen.
Psychological effects of alcohol questions
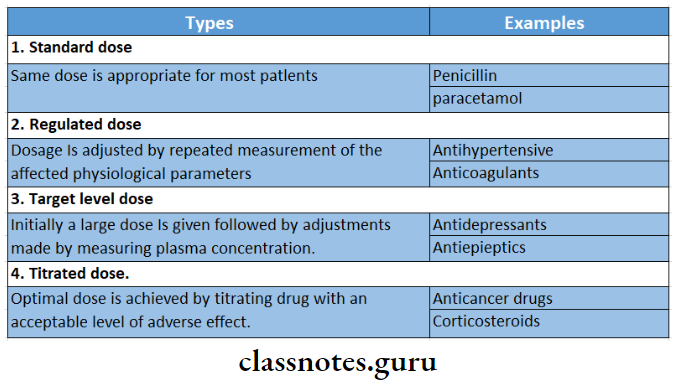
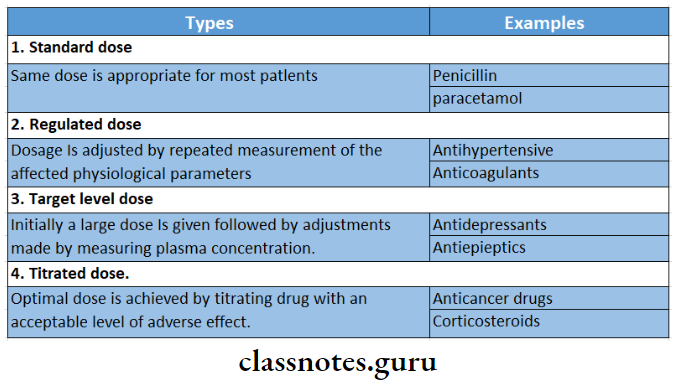
Question 6. Drug dosage.
Answer:
A dose is the appropriate amount of a drug needed to pro- duce a certain degree of response in a patient.
Viva Voce:
- Acidic drugs are rapidly absorbed from the stomach
- Most of the drugs are absorbed by passive diffusion
- Propranolol has extensive first-pass metabolism
- Drugs are eliminated from the body by first-order kinetics or zero-order kinetics