Antihypertensive Drugs Important Notes
1. Classification of antihypertensive drugs
- Drugs acting on the renin-angiotensin system
- Angiotensin-converting enzyme inhibitors
- Captopril
- Enalapril
- Lisinopril
- Ramipril
- Angiotensin 2 receptor antagonists
- Losartan
- Candesartan
- Olmesartan
- Renin inhibitor
- Aliskiren
- Sympatholytics
- Centrally acting – Clonidine, Methyldopa
- Ganglionic blockers – Trimethaphan
- Adrenergic neuron blocker – Guanethidine, reserpine
- Adrenergic receptor blocker
- Alpha blocker – prazosin, doxazosin
- Beta-blocker – propranolol, atenolol, esmolol
- Alpha and beta-blocker – atenolol, carvedilol
- Diuretics
- Thiazides – hydrochlorothiazides
- Loop diuretics – frusemide, torsemide
- Potassium-sparing diuretics – spironolactone, amiloride, triamterene
- Calcium channel blocker
- Verapamil, niofedipine, nicardipine, nimodipine
- Vasodilators
- Arteriolar dilators – hydralazine, minoxidil
- Arteriolar and venular dilators – sodium nitroprusside
Read And Learn More: Pharmacology Question and Answers
2. ACE inhibitors
- They are the first choice of drugs in all essential hypertension
- They are the most appropriate antihypertensives in patients with
- Diabetes
- Nephropathy
- Left ventricular hypertrophy
- Angina
- Post MI
- Advantage: lack of postural hypotension
- Most ACE inhibitors are prodrugs
- They need to be converted by hepatic osteolysis to active diacid metabolite
- ACE inhibitors that are prodrugs are
- Fosinopril
- Enalapril
- Benazepril
- Imidapril
- Perindopril
Classification of antihypertensive drugs
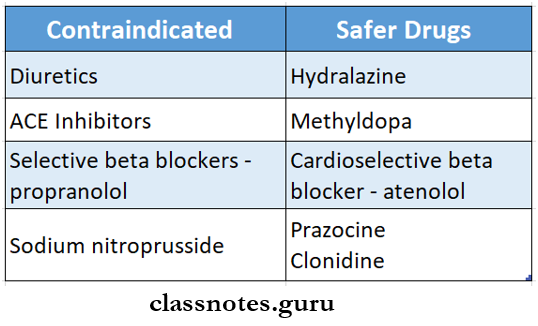
3. Antihypertensives and pregnancy
Antihypertensive Drug Long Essays
Question 1. Classify drugs used in the treatment of hypertension or antihypertensive drugs. State mechanism of action, indications, and adverse effects of any three of them
Answer:
Antihypertensive drugs:
- These drugs are used to lower BP in hypertension.
Antihypertensive drugs Classification:
1. Diuretics:
- Thiazides – hydrochlorothiazide, indapamide.
- High ceiling – Furosemide.
- K+ sparing – Spironolactone, Amiloride.
2. ACE inhibitors.
- Captopril, enalapril, Lisinopril, perindopril.
3. Angiotensin Antagonists.
- Losartan, candesartan.
4. Calcium channel blockers.
- Verapamil, diltiazem, Nifedipine, Felodipine.
5. β Adrenergic blockers
- Propranolol, Atenolol, Metoprolol.
6. β and α drenergic blockers.
- Labetalol, carvedilol.
7. α Adrenergic blockers.
- Prazosin, Terazosin, Doxazosin, Phentolamine.
8. Central sympatholytics.
- Clonidine, methyldopa.
9. Vasodilators.
- Hydralazine, sodium nitroprusside.
Diuretics:
Diuretics Mechanism of action:
1. Enhances sodium and water excretion.
↓
Decreases plasma and ECF volume.
↓
Decreases cardiac output
↓
Decreases BP.
↓
2. Increased excretion of sodium and water
↓
Decreases body sodium
↓
Relaxation of vascular smooth muscle.
↓
Decreases peripheral vascular resistance.
↓
Reduces BP.
Diuretics Use:
- In uncomplicated mild to moderate hypertension.
Diuretics Adverse effects:
- Hypokalemia.
- Carbohydrate intolerance.
- Fatigue, loss of energy.
- Impotence.
- Hyperlipidaemia, hyperuricemia.
- Decreased libido.
Pharmacology of antihypertensive drugs
Vasodilators – Hydralazine:
- Mechanism of action:
1. Arteriolar dilatation.
↓
Reduces vascular resistance
↓
Reduces BP.
↓
2. Compensatory mechanism.
Evoke tachycardia.
↓
Increases cardiac output and renin release.
↓
Increases aldosterone.
↓
Causes sodium and water retention.
↓
Decreases BP.
Vasodilators – Hydralazine Uses:
- Moderate to severe hypertension.
- Low doses are added to diuretics and β blockers.
- Only antihypertensive drugs are used in pregnancy.
Vasodilators – Hydralazine Adverse effects:
- Flushing, headache, dizziness, palpitation.
- Precipitate angina.
- Paraesthesia, tremor, muscle cramps.
- Rheumatoid arthritis.
ACE – Inhibitors:
- Mechanism of action:
Prevent formation of angiotension 2 and aldosterone.
↓
Causes vasodilation.
↓
Peripheral vascular resistance disease.
↓
BP decreases.
ACE – Inhibitors Uses:
- Hypertension.
- Myocardial infarction.
- Coronary artery disease.
- Chronic renal failure.
- Scleroderma renal crisis.
ACE – Inhibitors Adverse effects:
- Persistent dry cough.
- Angioneurotic edema.
- Hypotension.
- Hyperkalemia.
- Skin rashes
- Teratogenicity
- Others – headache, nausea, abdominal pain, proteinuria, neutropenia.
Question 2. Discuss the pharmacological actions, uses, and adverse effects of angiotensin-converting enzyme inhibitors – ACE inhibitors.
Answer:
ACE-Inhibitors:
ACE-Inhibitors Actions:
1. On Renin-Angiotensin system.
- Angiotensin 1 is converted into angiotensin 2 by angiotensin converting enzyme.
- Thus, if this enzyme is inhibited by ACE inhibitors, it prevents the formation of angiotensin 2.
- This further prevents the formation of aldosterone.
- This leads to vasodilation and a decrease in peripheral vascular resistance.
2. On Bradykinin level.
- ACE inhibitors raise bradykinin levels, which is a potent vasodilator.
- This causes a fall in B.P.
3. On vital organs.
- By selective vasodilation, ACE inhibitors increase blood flow to vital organs.
ACE-Inhibitors Uses:
1. Hypertension
- ACE inhibitors are first-line drugs for hypertension.
- Used in all grades of hypertension.
- Combining it with diuretics increases its efficacy.
- It can be used in hypertensive patients along with the following diseases.
- Left ventricular failure
- Diabetics
- Renal diseases.
- Co-existing ischaemic heart disease.
2. Congestive cardiac failure (CCF)
- ACE inhibitors cause arteriolar and vasodilatation in it
- This reduces preload and afterload.
3. Myocardial infarction.
- ACE inhibitors reduce early as well as long-term mortality.
4. Prophylaxis in high cardiovascular-risk patient
- Protects myocardium and vasculature.
5. Diabetic nephropathy.
- Prolonged use of ACE-inhibitor prevents or delays end-stage renal disease.
6. Scleroderma crisis.
- The life-saving drug in it
Hypertension treatment pharmacology questions
Question 3. Classify antihypertensive agents. Discuss the pharmacological actions, uses, and adverse effects of calcium channel blockers.
Answer:
Classification of Antihypertensive Drugs:
- Drugs acting on the renin-angiotensin system
- Angiotensin-converting enzyme inhibitors
- Captopril
- Enalapril
- Lisinopril
- Ramipril
- Angiotensin 2 receptor antagonists
- Losartan
- Candesartan
- Olmesartan
- Renin inhibitor
- Aliskiren
- Angiotensin-converting enzyme inhibitors
- Sympatholytics
- Centrally acting – Clonidine, Methyldopa
- Ganglionic blockers – Trimethaphan
- Adrenergic neuron blocker – Guanethidine, reserpine
- Adrenergic receptor blocker
- Alpha blocker – prazosin, doxazosin
- Beta-blocker – propranolol, atenolol, esmolol
- Alpha and beta-blocker – labetalol, carvedilol
- Diuretics
- Thiazides – hydrochlorothiazides
- Loop diuretics – frusemide, torsemide
- Potassium-sparing diuretics – spironolactone, amiloride, triamterene
- Calcium channel blocker
- Verapamil, niofedipine, nicardipine, nimodipine
- Vasodilators
- Arteriolar dilators – hydralazine, minoxidil
- Arteriolar and venular dilators – sodium nitroprus- side
Calcium Channel Blockers (CCB) Actions:
1. Action on smooth muscle
- Vascular smooth muscle
- Relaxation of arteriolar smooth muscle reduced peripheral vascular resistance → reduction in blood pressure
- Other smooth muscle
- Relaxation of GIT and bronchial smooth muscles
- Relaxes the uterus which is useful in preterm labor
2. Action on heart
- Depresses myocardial contractibility
- Reduces heart rate
- Reduces cardiac work
3. Action on coronary circulation
- Dilates coronary vessels
- Increases coronary blood flow
Calcium Channel Blockers (CCB) Uses:
- Angina pectoris
- CCB reduces the frequency and severity of angina
- Hypertension
- Arrhythmias
- Verapamil controls ventricular rate in atrial flatter or fibrillation
- Peripheral vascular disease
- Used in Raynaud’s disease for its vasodilator effects
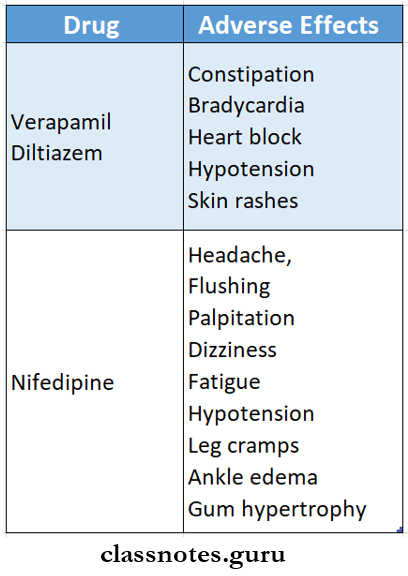
Calcium Channel Blockers (CCB) Adverse Effects:
Drugs for hypertension short notes
Antihypertensive Drugs Short Essays
Question 1. Captopril.
Answer:
Captopril is an orally active dipeptide ACE inhibitor.
- It is a sulfhydryl-containing dipeptide.
Captopril Mechanism of Action:
- Prevents the formation of Angiotensin 2 and aldosterone.
- Increases bradykinin levels.
- Causes vasodilation and fall of BP.
- Both systolic and diastolic BP decreases.
- It has no action on cardiac output.
Captopril Pharmacokinetics:
- Orally administered.
- About 70% of the drug is absorbed.
- The plasma half-life is approx. 2 hours.
- Duration of action – 6 -12 hours.
Captopril Adverse effects:
- Hypotension.
- Hyperkalemia.
- Cough.
- Rashes, urticaria.
- Angioedema.
- Loss of alteration in taste sensation.
- Fetal growth retardation.
- Headache, dizziness, nausea.
- Acute renal failure.
- Granulocytopenia.
Question 2. Calcium channel blockers are used in the treatment of hypertension.
Answer:
Calcium channel blockers used in the treatment of hypertension include.
1. Phenylalkylamines – Verapamil.
2. Benzothiazepines – Diltiazem.
3. Dihydropyridines – Nifedipine, felodipine, Amlodipine, Lacidipine, Nimodipine.
- These drugs are well-tolerated and effective.
- They dilate arterioles resulting in reduced peripheral vascular resistance.
- Effective in elderly patients.
- Can be used alone or in combination with other an¬tihypertensive drugs.
- Nifedipine produces some reflex tachycardia.
- Fluid retention is negligible.
- Short-acting drugs are associated with increased mortality and risk of sudden death.
- They are used in patients with angina.
- Not preferred in patients who also have left ventricu¬lar hypertrophy and previous myocardial infarction.
- They are used for short periods for smoother control of BP.
- Nifedipine is administered sublingually and is used for hypertensive emergencies.
- It effectively lowers BP in 10 min.
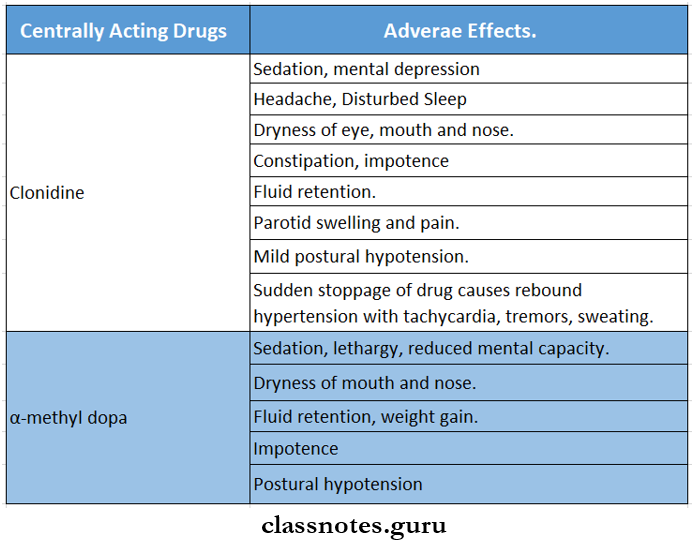
Question 3. Mention two centrally acting antihypertensive drugs and mention their adverse effects.
Answer:
Combination therapy in hypertension pharmacology
Question 4. The rationale of using clonidine in hypertension.
Answer:
Clonidine is an imidazoline derivative.
it is a partial agonist with high affinity and high intrinsic activity at α2 receptors.
Clonidine in Hypertension Action:
1. Stimulation of α2 receptors in the medulla.
↓
Decreases central sympathetic outflow.
↓
Blocks the release of noradrenaline from the nerve terminal.
↓
Results in fall in BP and bradycardia.
2. Clonidine active specific imidazoline receptors in the brain.
- This causes a fall in BP.
Pharmacokinetics:
- Effective orally.
- Plasma half-life – 8 -12 hours.
- The effect lasts for 6 – 24 hours.
Question 5. The rationale of using p-blockers in hypertension.
Answer:
Beta-blockers used in hypertension are propranolol, atenolol, esmolol, and metoprolol.
- They are effective and well-tolerated.
- They are mild antihypertensive.
- They reduce cardiac output and lowers plasma renin activity.
- This reduces BP.
- They can be used alone or in combination with other antihypertensive.
- Beta-blockers should always be tapered while with-drawing.
- They can be used in patients with angina and cardiac arrhythmia.
- Esmolol is used in intraoperative and postoperative hypertension and in hypertensive emergencies.
- It is used better than other antihypertensive drugs because of.
1. Absence of postural hypotension.
2. Absence of bowel alteration.
3. Absence of salt and water retention.
4. Less side effects.
5. Low cost
Antihypertensive Drugs Short Answers
Question 1. Clonidine.
Answer:
Clonidine is an imidazoline derivative.
- It is a selective α2 -agonist
Clonidine Mechanism:
Stimulation of α2 receptors.
↓
Decreases central sympathetic outflow.
↓
Blocks release of noradrenaline.
↓
Resulting in a fall in BP.
Clonidine Uses:
- Hypertension.
- Opioid withdrawal syndrome.
- Postoperative epidural analgesia.
- Menopausal syndrome.
Question 2. Reserpine.
Answer:
Reserpine is an alkaloid obtained from Rauwolfia serpentina.
Reserpine Mechanism:
Destruction of vesicles in the adrenergic neurons.
↓
Depletion of monoamines like noradrenaline, dopamine, and 5-HT.
↓
Reduces BP.
Reserpine Uses:
- Hypertension.
- Psychosis.
Question 3. Mention two uses and two adverse effects of thiazide.
Answer:
Thiazide Uses:
- Mild hypertension.
- Congestive heart failure.
- Hepatic or renal edema.
- Renal stones
- Diabetes insipidus.
Thiazide Adverse effects:
- Hypokalemia.
- Hyperglycaemia.
- Hyperuricaemia.
- Hyperlipidaemia.
- Impotence.
- Decreased libid
Question 4. Enaiapril.
Answer:
Enalapril is an angiotensin-converting enzyme inhibitor.
- It is a prodrug, thus it has to be converted in the body to the active form.
- Hence it acts slowly.
Enaiapril Uses:
- Hypertension
- Congestive cardiac failure.
- Myocardial infarction.
Enaiapril Adverse effects:
- Persistent dry cough.
- Hyperkalaemia.
- Taste alteration.
Side effects of antihypertensive drugs MCQs
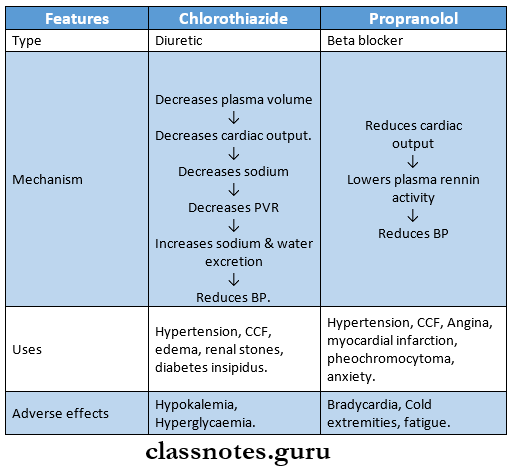
Question 5. Chlorothiazide diuretics used in hypertension.
Answer:
Chlorothiazide is a thiazide diuretic that is used in the treatment of mild hypertension.
Mechanism:
Decreases plasma volume
↓
Decreases cardiac output.
↓
Decreases sodium
↓
Decreases peripheral vascular resistance (PVR)
↓
Increases sodium and water excretion
↓
Reduces BP.
- Thiazides cause hypokalaemia and hence they are used with potassium-sparing diuretics.
Question 6. Advantages of ACE inhibitors over other anti-hypertensive drugs.
Answer:
ACE inhibitors have the following advantages.
- Lack of postural hypotension, electrolyte disturbances, feeling of weakness, and CNS effects.
- Safer in asthmatics, diabetics, and peripheral vascular disease patients.
- Reverse left ventricular hypertrophy.
- No hyperuricemia, no harmful effect on plasma lipid profile.
- No rebound hypertension on withdrawal.
- Minimum worsening of quality of life.
Question 7. Compare chlorothiazide and propanoiol.
Answer:
First-line treatment for hypertension
Question 8. Mention two ACE inhibitors and two calcium channel blockers.
Answer:
- ACE inhibitors: Captopril, Enalapril, Lisinopril
- Calcium channel blockers: Verapamil, Diltiazem, Nifedipine.
Question 9. Enlist two Angiotensin receptor blockers and write the mechanism of action.
Answer:
Mechanism of Action:
- Blocks angiotensin 1 receptor
- Relaxes vascular smooth muscles
- Promotes salt and water excretion
- Reduces plasma volume
Examples:
- Losartan, candesartan, irbesartan
Antihypertensive Drugs Viva Voce:
- Sodium nitroprusside is arteriolar and venous dilator
- Hydralazine is arteriolar dilator
