Diabetes Mellitus Important Notes
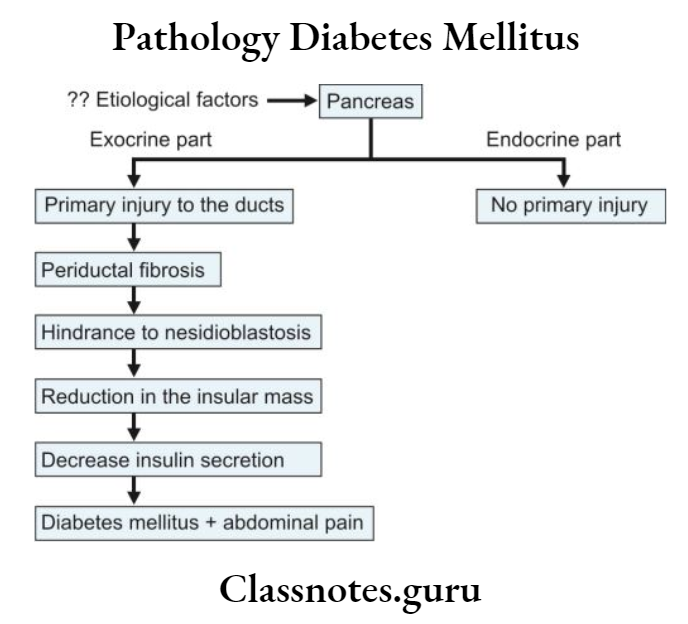
1. Etiology of Diabetes Mellitus
- Reduced insulin secretion
- Decreased glucose use by the body
- Increased glucose production
2. Complications of Diabetes Mellitus
- Ketoacidosis
- Nonketotic coma
- Hypoglycemia
- Atherosclerosis
- Nephropathy
- Neuropathy
- Microangiopathy
- Retinopathy
- Infections
Diabetes Mellitus Long Essays
Question 1. Define diabetes mellitus. Discuss laboratory diagnosis and complications of diabetes mellitus.
Answer:
Diabetes Mellitus Definition: Diabetes mellitus is defined as a heterogenous metabolic disorder characterized by the common feature of chronic hyperglycaemia with disturbance of carbohydrate, fat and protein metabolism
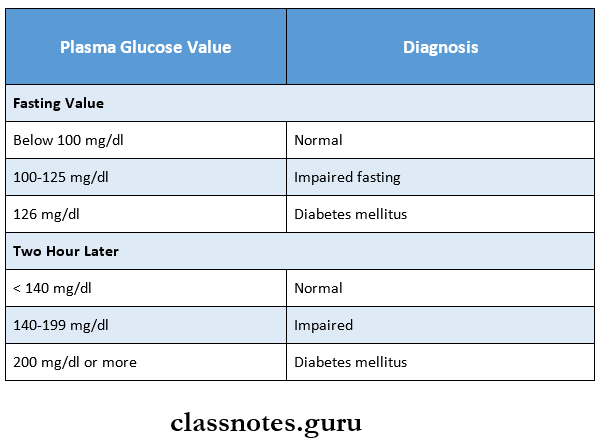
Diabetes mellitus Laboratory Diagnosis:
- Urine testing
- Glucosuria
- The Dipstick method is used
- In this method, enzyme coated paper strip is used which turns purple when dipped in urine containing glucose
- ketonuria
- Rothera’s test is used to detect ketone bodies in urine
- Glucosuria
- Single blood sugar estimation
- O-toluidine, Somogyi-Nelson and glucose oxidase methods are used
- A fasting plasma glucose value above 126 mg/dl is certainly indicative of diabetes
- Screening by fasting glucose test
- It is a screening test for type 2 diabetes mellitus
- Done for individuals above 45 years
- Oral glucose tolerance test
Read And Learn More: Pathology Question And Answers
Diabetes Mellitus Method:
- Intake of a high carbohydrate diet 3 days prior to the test
- Overnight fasting on the day of the test
- A fasting blood sugar sample is collected
- 75 gms of glucose dissolved in 300 ml of distilled water is given to the individual
- Blood and urine samples are collected at half-hour intervals for atleast 2 hours
Diabetes Mellitus Result:
Diabetes Mellitus Complications:
- Acute metabolic complications
- Diabetic ketoacidosis
- Develop in patients with severe insulin deficiency
- Pathogenesis
- Diabetic ketoacidosis
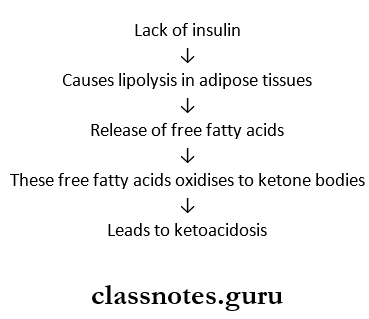
- Diabetic ketoacidosis Clinical Features:
- Nausea, vomiting, anorexia
- Deep and fast breathing
- Mental confusion
- Coma
- Diabetic ketoacidosis Clinical Features:
- Hyperosmolar hyperglycaemia non-ketotic coma
- It is a complication of type 2 diabetes mellitus
- Caused by severe dehydration which leads to sustained hyperglycaemia diuresis
- Hyperglycaemia non-ketotic coma Clinical Features:
- High blood sugar
- High plasma osmolality
- Thrombotic and bleeding complications
- Hyperglycaemia non-ketotic coma Clinical Features:
- Hypoglycaemia
- Develop in type 1 diabetes mellitus
- Occurs due to
- Excessive administration of insulin
- Missing a meal
- Stress
- It produces
- Permanent brain damage
- Worsening of diabetic control
- Rebound hyperglycaemia
- Late systemic complications
- Atherosclerosis
- Common in both type 1 and type 2 diabetes mellitus
- Its contributory factors are
- Hyperlipidaemia
- Reduced HDL levels
- Non-enzymatic glycosylation
- Increased platelets adhesiveness
- Obesity
- Hypertension
- Atherosclerosis may lead to
- Myocardial infarction
- Cerebral stroke
- Gangrene of toes and feet
- Diabetic microangiopathy
- It is the basement membrane thickening of small blood vessels and capillaries of different organs and tissues
- Occurs due to increased glycosylation of haemoglobin and other proteins
- Diabetic nephropathy
- It is a severe complication of diabetes mellitus
- Occurs in both types
- Diabetic nephropathy Features:
- Asymptomatic proteinuria
- Nephrotic syndrome
- Progressive Renal failure
- Hypertension
- Diabetic nephropathy Features:
- Diabetic neuropathy
- Effects all parts of the nervous system
- Pathological Changes:
- Segmental demyelination
- Schwann cell injury
- Axonal damage
- Pathological Changes:
- Effects all parts of the nervous system
- Diabetic retinopathy
- It is the cause of blindness
- Other retinal complications include
- Glaucoma
- Cataract
- Corneal disease
- Infections
- Diabetic patients are more susceptible to infections like tuberculosis, pyelonephritis, otitis, carbuncles and diabetic ulcers
- Atherosclerosis
Diabetes Mellitus Short Essays
Question 1. Aetiopathogenesis of Diabetes Mellitus.
Answer:
1. Genetic susceptibility Diabetes mellitus involves inheritance of multiple genes
2. Autoimmune factors
- Presence of islet cell antibodies against insulin
- Occurrence of CD8+ T lymphocytes with a variable number of CD4+ T lymphocytes and macrophages
- Selective destruction of beta cells by T-cell mediated cytotoxicity or by apoptosis
3. Constitutional factors
- Obesity, hypertension and level of physical activity
- Presence of viral infection
4. Insulin resistance
- It leads to
- Impaired glucose uptake by tissues
- Increased glucose synthesis by the liver
- Hyperglycaemia
5. Impaired insulin secretion
- In diabetes mellitus, initially, there is increased secretion of insulin
- Later beta cells fail to secrete adequate insulin
6. Increased hepatic glucose synthesis
- In diabetes mellitus gluconeogenesis process remains unaffected
- Thus there is increased glucose synthesis in the liver.
Diabetes Mellitus Short Question And Answers
Question 1. Glycosuria.
Answer:
- It is the condition of glucose excretion in urine.
- Glucose appears in urine when the plasma glucose concentration exceeds the renal threshold for glucose.
Glycosuria Types:
1. Renal glycosuria.
- It is a benign condition.
- Occurs due to a reduced renal threshold for glucose.
- It is unrelated to diabetes.
2. Alimentary glycosuria.
- In certain individuals, blood glucose rapidly Increases after meals which get excreted in the urine.
- This is known as alimentary glycosuria.
- It is observed in.
- Normal individuals.
- Individuals with.
- Hepatic diseases
- Hyperthyroidism
- Peptic ulcer.
